Most Common Teeth Diseases
Diseases of the Teeth
Diseases can affect any organ in our body. Our teeth are no exception. When it comes to teeth, we need to understand that the infection can spread across the surrounding structures and eventually impact other organs in our body. And since not all teeth diseases hurt, we may not even know that there is a problem. Let’s look at the most common tooth diseases.
Cavities – Tooth Decay
Almost everyone has had a cavity or more in their lifetime. And that is because we love sweets. Plus, we may not be the best when it comes to brushing and flossing. The bacteria causing tooth decay use the sweets and plaque as fuel. The more sweets we eat and the more plaque we leave on our teeth, the more active these bacteria become.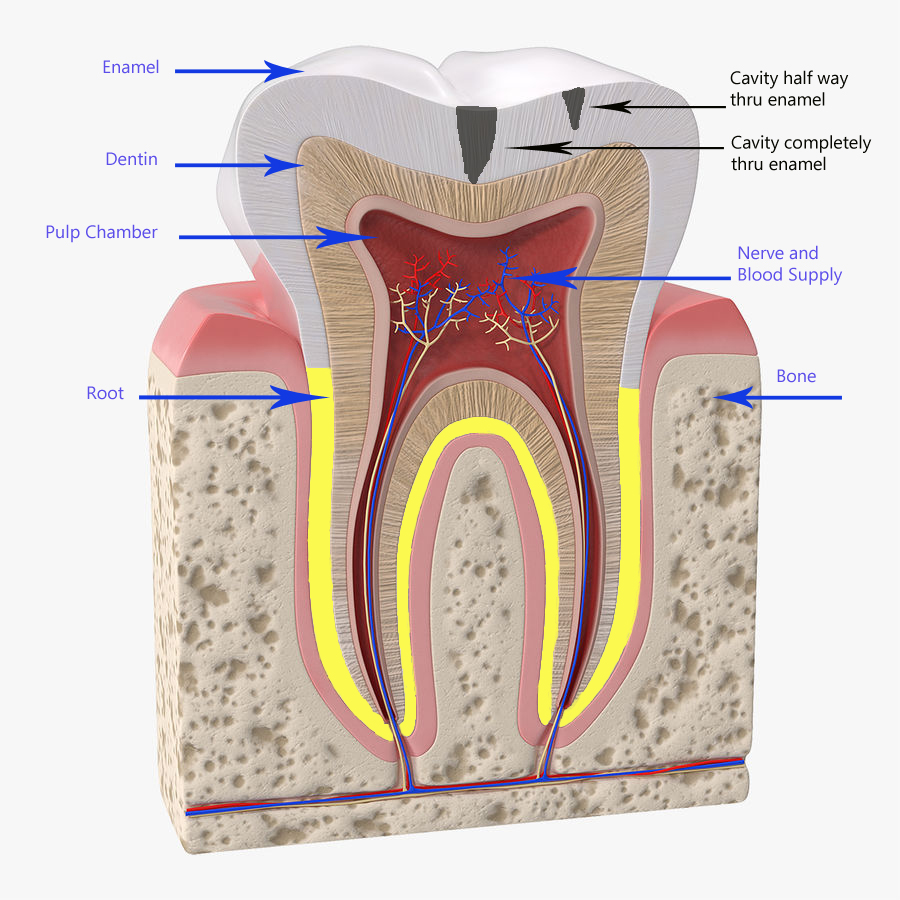
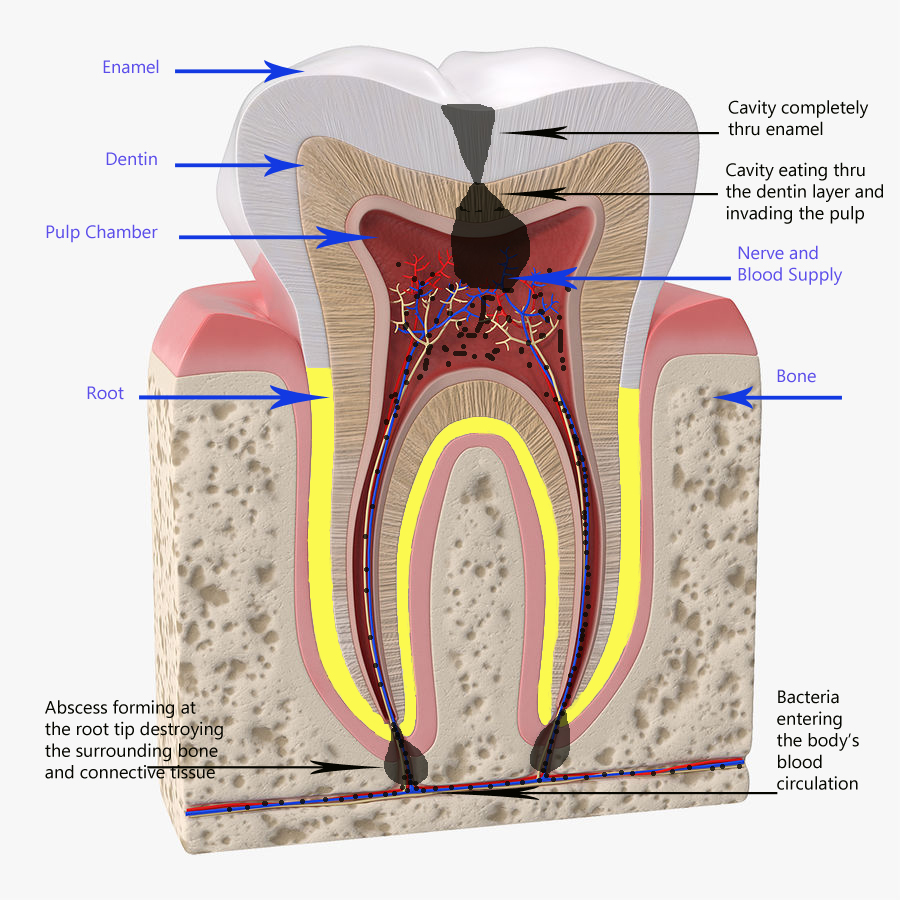
Enamel contains no nerve endings. The enamel layer is on average 2-3 mm thick. Since the decay eats at the enamel layer very slowly, it will be a while before you “feel” anything.
Once the tooth decay reaches the dentin junction, that’s when you start feeling like you have a cavity. Sensitivity and pain to sweets and cold are two common symptoms of a tooth cavity that has reached the dentin layer.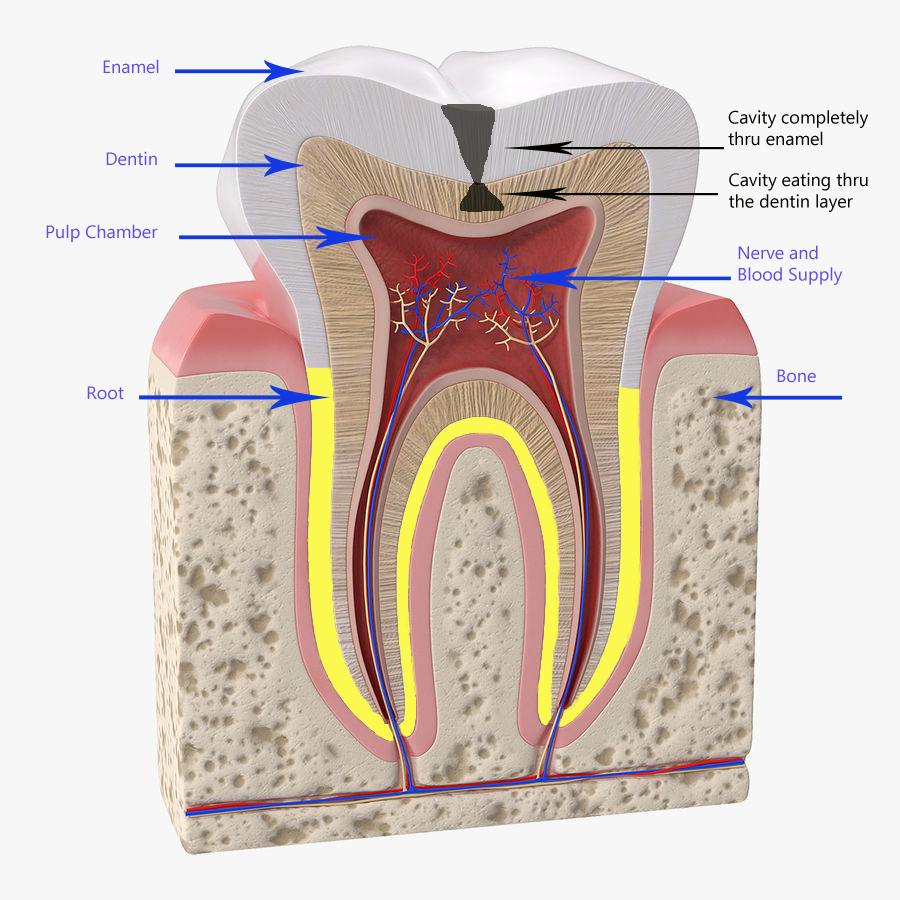
The dentist can fix a cavity when it is small quite easily. However, delaying the treatment results in the cavity growing bigger. The reason is that the cavity doesn’t stop growing once it reaches the dentin. Tooth decay can extend into the nerve and the blood supply.
Abscessed Tooth – Infection in Blood
A tooth’s cavity grows at different rates depending on what the patient eats and their dental hygiene. The layer where the cavity is located also makes a difference in how rapidly the cavity gets bigger. A cavity in the enamel layer grows slower compared to dentin. And the reason is the chemical structure of enamel is more impervious to decay than dentin’s chemical makeup.
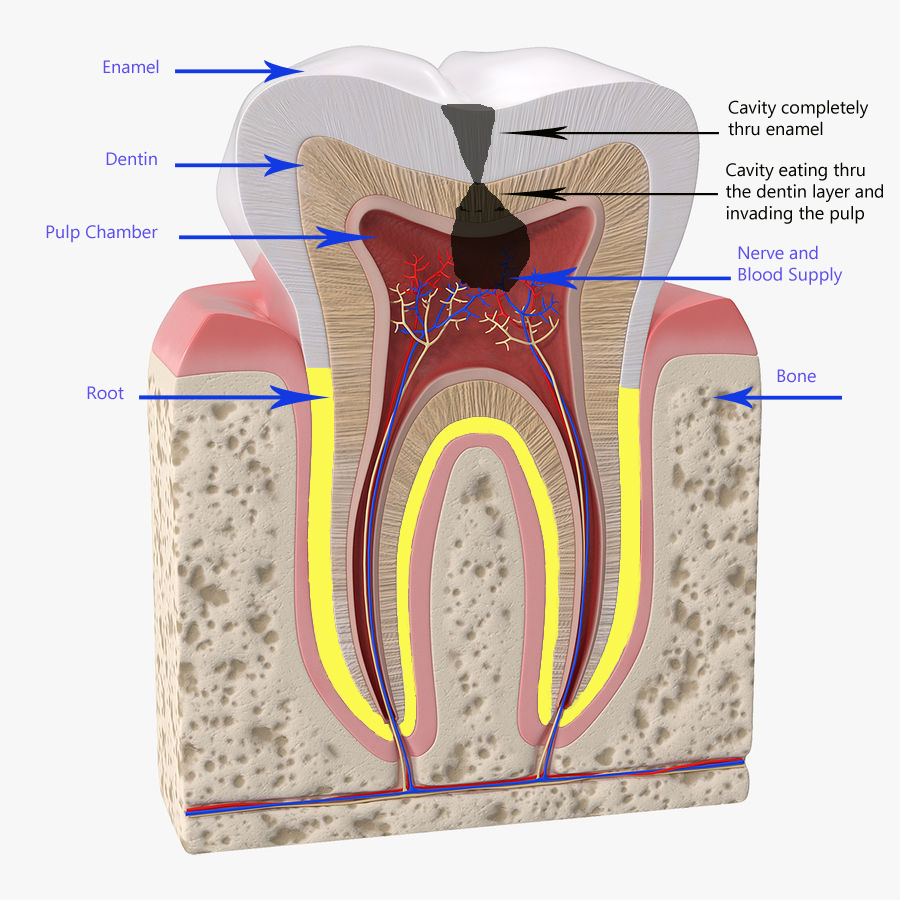 Once the decay reaches the nerve, the bacteria can enter the bloodstream causing an infection. A tooth that has nerve damage becomes sensitive to heat. As the nerve damage progresses, the tooth starts throbbing and even causes sleeping problems. Pain while chewing is also common at this stage.
Once the decay reaches the nerve, the bacteria can enter the bloodstream causing an infection. A tooth that has nerve damage becomes sensitive to heat. As the nerve damage progresses, the tooth starts throbbing and even causes sleeping problems. Pain while chewing is also common at this stage.
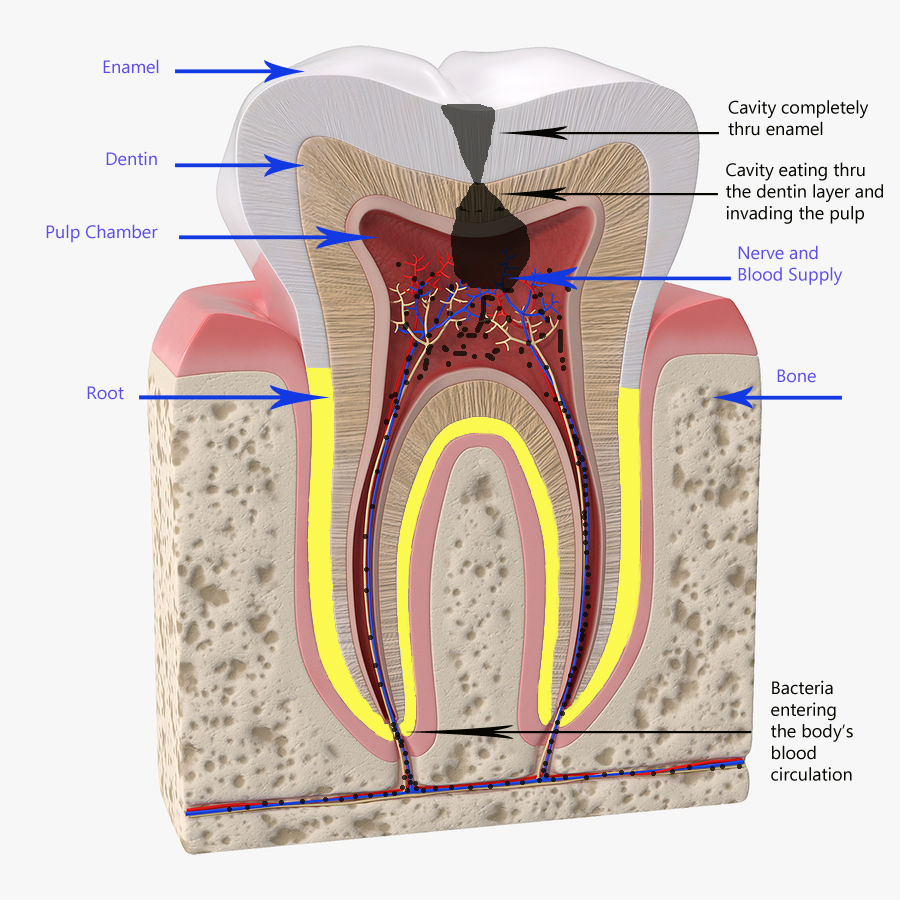 When bacteria enter our bloodstream, it leads to the development of an infection. We first develop a localized fever, redness, inflammation, and aches. If left untreated, the swelling will keep growing.
When bacteria enter our bloodstream, it leads to the development of an infection. We first develop a localized fever, redness, inflammation, and aches. If left untreated, the swelling will keep growing.
Sometimes this swelling gets so severe that it causes breathing difficulties by placing pressure against the airway. And as the number of bacteria increase, our body enters a state of septic shock. At this stage, we have a real medical emergency. Compromised airways or infected blood don’t go away with aspirin or a filling.
Tooth cavities and decay attack the tooth itself. Other tooth diseases affect the supporting structures of the tooth.
Gingivitis – Gum Disease
The teeth and the jaw bone are not fused. Instead, teeth are attached to the jaw bone by a thin layer of connective tissue. A cavity attacks the tooth structure. In contrast, gum disease attacks this connective tissue, not the tooth itself.
In tooth decay, the bacteria release acids that destroy the enamel and cause the cavity to form. Whereas in gum disease, the bacteria cause our body to initiate a defensive immune response, which results in damage to the gums and the connective tissue.
The disease of the tooth’s supporting structures eventually leads to the loss of the tooth. You can think of gum disease as soil erosion around a tree. When the soil decline gets severe enough, the tree falls. And much like the tree example, this damage doesn’t happen overnight. Learning how to clean the teeth properly is the best defense against gum disease.
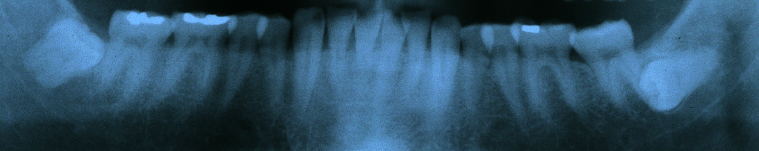
Periodontal Disease – Infected Gums – Gum Abscess
Periodontal disease results from untreated gingivitis. And what separates the two is the damage to the foundation of the tooth. With gingivitis, the damage is only to the gum tissue around the tooth. With periodontitis, the damage extends further into the bone and down to the connective tissue. Teeth look longer as the gums pull away. Gums bleed and are generally tender. Some teeth will become noticeably looser. And there will come a time when the teeth are so wiggly that nothing can save them.
 Gum abscess can occur during periodontitis. What happens is that the infection and pus keep building up underneath the gums. Since the pus is growing in a closed space and can’t drain away, the pus volume keeps increasing. The buildup of this infection causes the gums to bulge out as a result of the pressure.
Gum abscess can occur during periodontitis. What happens is that the infection and pus keep building up underneath the gums. Since the pus is growing in a closed space and can’t drain away, the pus volume keeps increasing. The buildup of this infection causes the gums to bulge out as a result of the pressure.
Gum disease leads to tooth loss. The disease is also tied to other systemic ailments like heart disease, diabetes, and pregnancy complications. Gums disease starts with the formation of plaque on the teeth. When the patient doesn’t remove the plaque, the gums start getting out of control.
Impacted Teeth
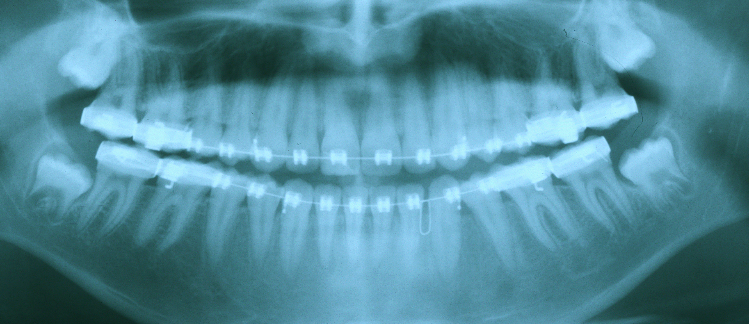
Baby teeth erupt into the mouth in a specific sequence. They then are replaced by adult teeth over the years. The specific eruption pattern helps the jaw bones to grow and develop to their standard size. However, sometimes a baby’s tooth becomes so severely decayed that your dentist removes it. When that happens, the growth of the jaw is compromised. As is often the case, the neighboring teeth start collapsing into the newly vacated space. The dental collapse leads to a physical blockage to the eruption path of the adult teeth. Consequently, the adult tooth then becomes trapped or impacted. But this is not the only way teeth get impacted.
At times, the jaw doesn’t grow enough to accommodate all of the adult teeth. Wisdom teeth are the last set of teeth that come into the mouth. As such, there may not be enough room left for them to come in straight. It is not uncommon to see the wisdom teeth tipping forward and jamming up against the front tooth. These teeth often cause pain and discomfort to the patient and need to be removed.
Missing Teeth
 Our genetic code is responsible for the creation of our organs, including our teeth. If the genes are missing or altered somehow, the teeth made by those genes will be affected. Sometimes teeth turn out misshapen, and at times the teeth are completely missing. Our upper front side teeth are typically the ones that are affected by this congenital condition. The missing teeth often impact the smile negatively.
Our genetic code is responsible for the creation of our organs, including our teeth. If the genes are missing or altered somehow, the teeth made by those genes will be affected. Sometimes teeth turn out misshapen, and at times the teeth are completely missing. Our upper front side teeth are typically the ones that are affected by this congenital condition. The missing teeth often impact the smile negatively.
Other Dental Diseases
There are many other diseases of the teeth. Here, we talked about some of the major ones. For more on common dental diseases, check out this cool article on WebMD.
Teeth Diseases – Multiple Solutions
The dentist can treat and correct the disease affecting the teeth in many ways. Tooth bondings, white fillings, root canal therapy, crowns, dental implants, and dental bridges are a few ways the dentist can help the patient. Our dentist, with over 20 years of experience, can treat all of these conditions. If you or a loved one is suffering from a tooth disease, contact us, and we’ll schedule a consultation with the doctor for you.

 When a tooth is badly injured, treatment choices become limited. A badly damaged tooth can often be saved with a
When a tooth is badly injured, treatment choices become limited. A badly damaged tooth can often be saved with a 
